Diabetes affects many parts of the body, but one serious and lesser-known complication occurs in the eyes. Diabetic Macular Edema (DME) is a major cause of vision loss in people with diabetes. Understanding this condition can help with early detection, timely treatment, and preventing long-term vision problems. This guide by Dr Maneesh Dhupper explains what diabetic macular edema is, why it occurs, its symptoms, treatment options, and preventive care.
What Is Diabetic Macular Edema?
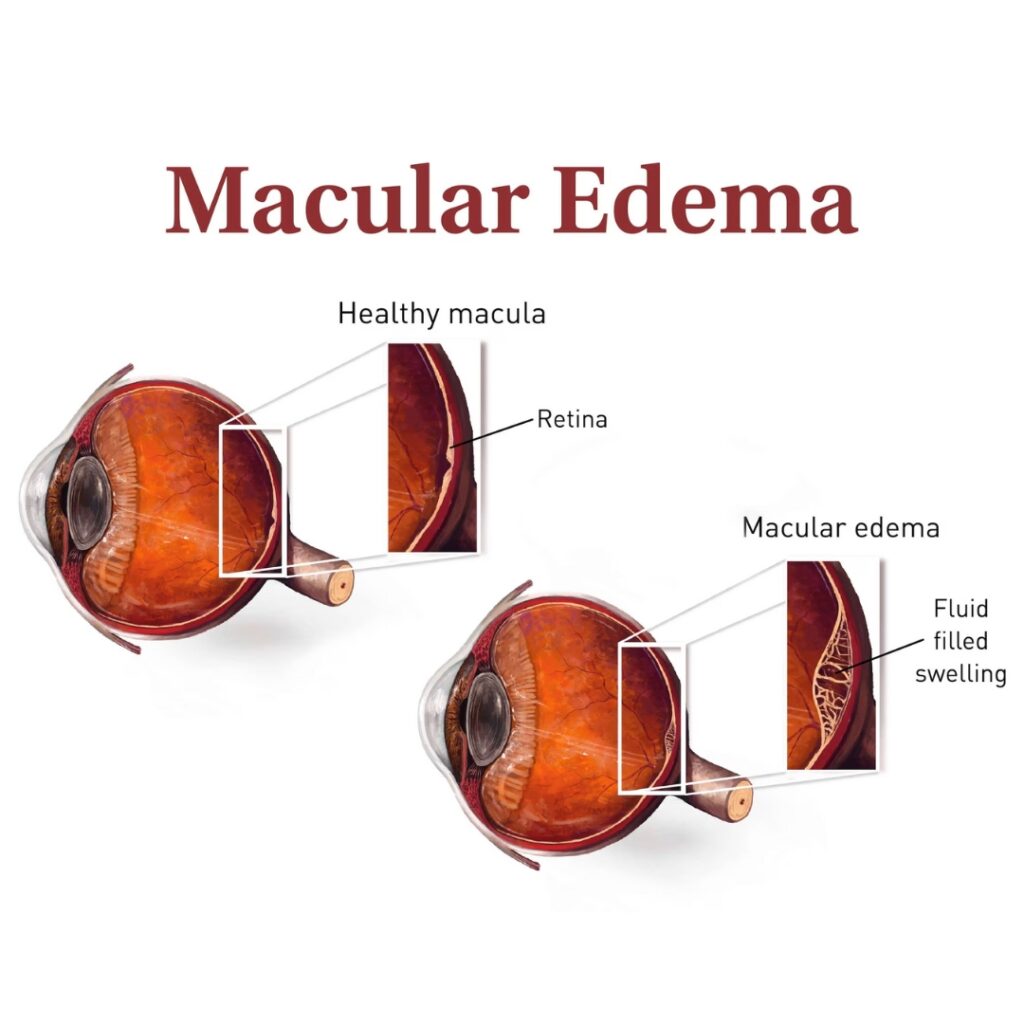
Diabetic Macular Edema is a complication of diabetic retinopathy, which is caused by prolonged high blood sugar that damages the tiny blood vessels in the retina. The macula, which is the central part of the retina responsible for sharp, detailed vision, swells due to fluid leakage from weakened blood vessels. This fluid buildup causes macular swelling, retinal thickening, and eventually results in distorted or blurred central vision.
DME can happen at any stage of diabetic retinopathy but is more common in advanced stages. If it goes untreated, the swelling can permanently damage the macula, leading to severe vision loss.
How Does Diabetic Macular Edema Develop?
To understand DME, it’s helpful to know the changes happening inside the retina:
1. Damage to Retinal Blood Vessels
High blood sugar harms retinal blood vessels, making them weak and leaky. These damaged areas can lead to microaneurysms, which are tiny balloon-like swellings on blood vessels. These are among the first visible signs of diabetic retinopathy.
2. Fluid Leakage & Retinal Thickening
As blood vessels leak fluid, the macula swells. This swelling thickens the retina, interfering with its ability to function properly.
3. Reduced Blood Supply
In many patients, decreased blood flow or macular ischemia, which is a lack of oxygen to the macula, also contributes to vision loss. When the macula doesn’t get enough oxygen, it cannot work effectively.
4. Progressive Vision Loss
Without medical help, the swelling increases and can lead to permanent damage.
Who Is at Risk of Developing DME?
Anyone with diabetes, whether Type 1 or Type 2, can develop diabetic macular edema. The risk increases with:
– A long duration of diabetes
– Poor blood sugar control
– High blood pressure
– High cholesterol levels
– Smoking
– Kidney disease
People with diabetic retinopathy are especially at high risk and should have regular retinal examinations.
Symptoms of Diabetic Macular Edema
DME often develops quietly, with no noticeable symptoms in the early stages. As the condition worsens, patients may notice:
– Blurred or wavy central vision
– Difficulty reading or recognising faces
– Faded or washed-out colours
– Dark or empty spots in the centre of vision
– Distortion in straight lines
If you experience any of these symptoms, it’s important to get an immediate evaluation from a retina specialist.
How Is Diabetic Macular Edema Diagnosed?
A thorough retinal examination is necessary for an accurate diagnosis. Specialists often perform:
– Fundus examination to check for microaneurysms and leakage
– Optical Coherence Tomography (OCT) to measure retinal thickness and macular swelling
– Fluorescein angiography to identify areas of leakage and macular ischemia
If you visit a retinal specialist like Dr. Manesh Dhupper (MBBS, MS Ophthalmology, Vitreo Retina Surgeon) at Gobind Nursing Home, these advanced diagnostic tools will help assess the condition.
Treatment Options for Diabetic Macular Edema
Modern treatments have greatly improved outcomes for patients with DME. The options include:
1. Anti-VEGF Injections
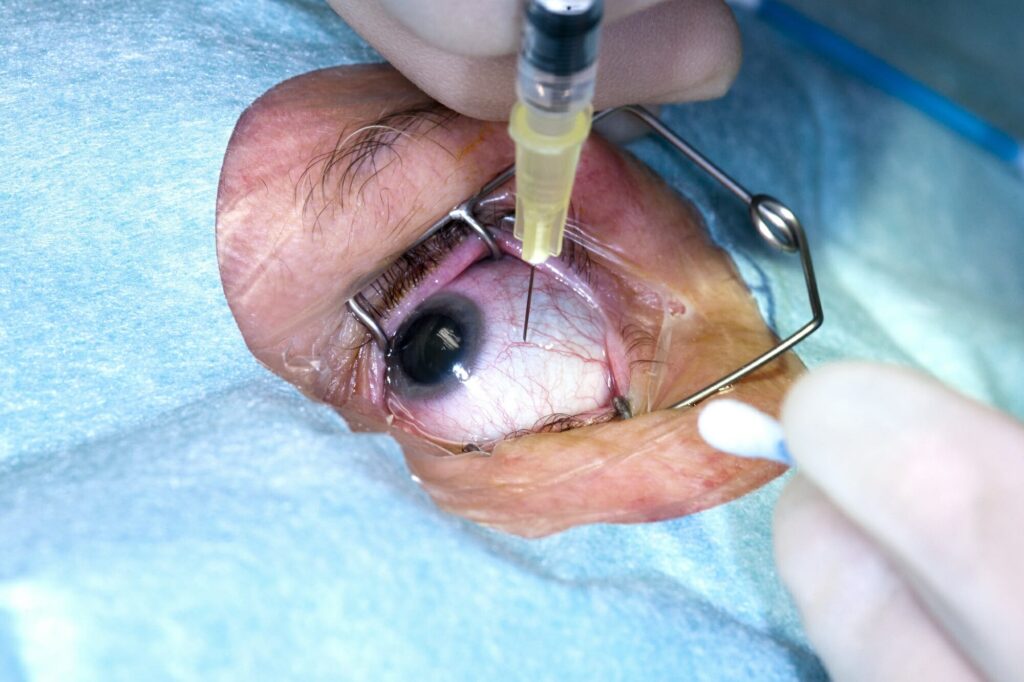
These injections block a protein called VEGF that causes abnormal blood vessel growth and leakage. Anti-VEGF therapy helps reduce macular swelling and improve vision in many cases.
2. Steroid Injections or Implants
Steroids reduce inflammation and are especially useful for patients who do not respond to anti-VEGF treatments. Long-acting steroid implants can provide sustained relief.
3. Laser Photocoagulation
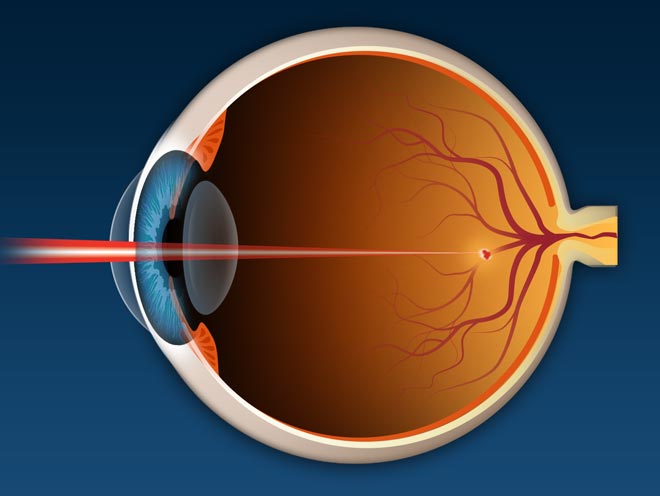
Laser treatment seals leaking blood vessels and prevents further fluid buildup. Although it may not fully restore lost vision, it is very effective in stabilising the condition.
4. Vitrectomy Surgery
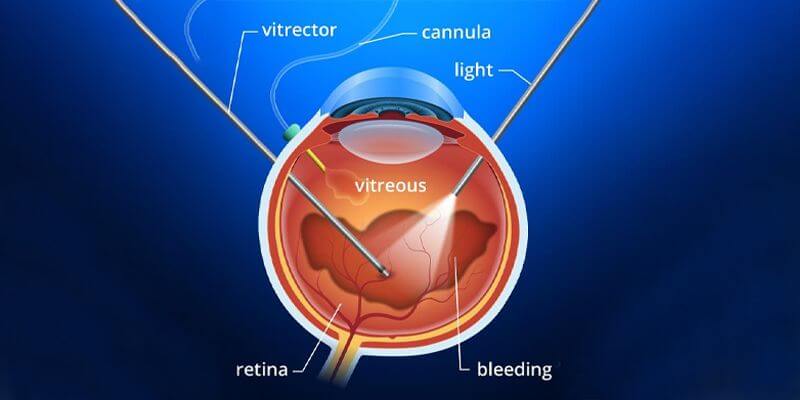
In advanced cases with significant bleeding or structural complications, surgery may be recommended. Retinal specialists like Dr. Manesh Dhupper perform these delicate procedures.
Prevention: Protecting Your Vision from DME
The best way to address diabetic macular edema is through prevention. You can significantly reduce your risk by:
– Maintaining stable blood sugar levels
– Controlling blood pressure and cholesterol
– Quitting smoking
– Eating a balanced, low-glycemic diet
– Exercising regularly
– Getting annual retinal checkups
Early detection is crucial. Many patients are unaware they have diabetic retinopathy or macular swelling until the damage is severe. Consulting an experienced retina specialist at the right time can save your vision.
Conclusion
Diabetic Macular Edema is a serious but treatable complication of diabetic retinopathy. With early diagnosis, proper medical care, and regular monitoring, patients can preserve their vision and prevent long-term complications. If you or a loved one has diabetes, do not ignore any change in vision. Seeking help from a qualified retina specialist, such as Dr. Manesh Dhupper, Vitreo Retina Surgeon at Gobind Nursing Home, can make a significant difference in managing this condition effectively.
Timely awareness and proactive care are your best defenses against diabetic eye disease.
Also Read:- Retinopathy of Prematurity (ROP): Causes, Symptoms, Prevention & Treatment

